Know your options
Time with your dermatologist can be limited. Thinking about what feeling free from psoriasis means to you, understanding your disease severity and knowing the different types of psoriasis treatments can help you get the most out of your consultation.
Use the Discussion Guide below to help you prepare for a meaningful conversation with your dermatologist.
1. Learn
What does a psoriasis-free feeling mean to you?
It is important to understand how psoriasis impacts your life and what you would like to achieve from your management plan. Make sure to discuss your goals with your dermatologist, so they can work with you to achieve them.
Feeling free from psoriasis could mean different things to different people. For example, it could mean:
![]() Reduced itching,
Reduced itching,
pain and discomfort
![]() Having great
Having great
relationships with
friends and family
![]() Sleeping well
Sleeping well
at night
![]() Less worry about
Less worry about
everyday activities,
such as going to the
supermarket
![]() Being able to
Being able to
concentrate at
work or school
![]() Wearing certain types
Wearing certain types
of clothes without
second-guessing
![]() Restored intimacy
Restored intimacy
with your partner
Share your goals with your dermatologist, and don’t worry if they evolve over time.
An important question to consider is – what you would do differently if you did not have psoriasis? You can think about this from a physical, mental or social perspective.
How severe is my psoriasis?
Understanding the severity of your condition is important to help determine
what management options may be appropriate.
Psoriasis severity can be measured in different ways. Each method is slightly different and considers different factors – some look at the physical impact (PASI and BSA), while others look at the impact on your quality of life (DLQI).
Originally a paper created by Cardiff University, the DLQI questionnaire has been transformed into a free app, providing easy access for both patients and HCPs.
DLQI: The official app was created and funded by Cardiff University* and is available on both Apple and Android Platforms.
Click on each scoring system to learn more:
PASI is a tool used to measure the severity and extent of psoriasis. A PASI score can range from 0 to 72 with a score of 5 to 10 being moderate and a score over 10 being severe.
Your dermatologist will take different points into consideration to calculate the severity:
- Location
The percentage area affected by psoriasis is evaluated in the four regions of the body:




Your dermatologist will look for psoriasis scales on each of these areas and assign a score of 0 to 6.
- Intensity
The intensity of your psoriasis is calculated based on:



The intensity of your psoriasis is then ranked with a score from 0 to 4.
BSA measures the amount of body surface area affected and the severity. It is still widely used in clinical practice.
Using the surface of the hand to equal 1% BSA, psoriasis is considered:
- Mild when less than 3% of the body is affected
- Moderate when 3%-10% of the body is affected
- Severe when more than 10% of the body is affected



The aim of DLQI questionnaire is to measure how much your psoriasis has affected your life and daily activities over the last week. It consists of 10 questions relating to symptoms, feelings, daily activities, leisure, work or school, personal relationships and treatment.
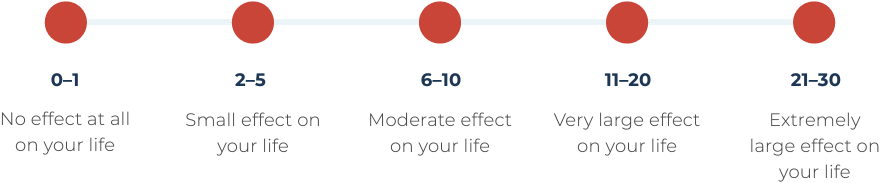
The final score, ranging from 0 to 30, will determine how psoriasis has affected your life based on the outcomes.
While the PASI and BSA tools are assessed with your dermatologist, you can complete the DLQI ahead of your appointment. Take two minutes to do the questionnaire before your next visit.
If you are not sure how severe your psoriasis is, speak with your dermatologist.
© Dermatology Life Quality Index. AY Finlay, GK Khan, April 1992. www.dermatology.org.uk
*AbbVie did not provide funding for and was not involved in the creation of this DLQI App or the DLQI questionnaire.
What are my
treatment options?
If your dermatologist decides to prescribe a treatment for your psoriasis, they will recommend the most suitable option for you.
Together, you and your dermatologist will create a personalised care plan based on the severity of your psoriasis, medical history and lifestyle.
- Mild Psoriasis
- Moderate to Severe Psoriasis
![]()
Topicals
Treatments that are applied directly to the plaques on the skin are called topicals. They can be available as creams, ointments, gels, shampoos or lotions.
The different types of topical treatments are:
- Emollients (moisturisers)
- Topical corticosteroids
- Combination products
- Vitamin D-like treatments
- Topical calcineurin inhibitors
- Salicylic acid
- Vitamin A treatments
- Coal tar preparations
Most topical treatments require a doctor’s prescription, but some may be available over-the-counter. They are generally prescribed as the first line of treatment.
When seeing a new doctor, discuss your current medications, including over-the-counter products, to avoid drug reactions and ensure your treatment plan stays on track.
Additionally, consider the cost of treatment options, as many are covered by the government’s Pharmaceutical Benefits Scheme (PBS). Consult your doctor or pharmacist to confirm if your medication meets the eligibility criteria for a subsidised price.
![]()
Light therapy
Light therapy, also called phototherapy, involves using controlled UVA or UVB rays along with a medication called psoralen (PUVA). This can help slow down the growth of skin cells in psoriasis-affected areas.
![]() Systemics
Systemics
Systemic treatments are prescription medications designed for people with varying degrees of psoriasis and disease severity.
These drugs work throughout the body and are suitable for those who don’t respond well to topical treatments or light therapy or can’t tolerate them.
![]() Biologics
Biologics
Biologics are a type of systemic treatment. They are made from living organisms, like cells or proteins, and can be given as injections or infusions.
When seeing a new doctor, discuss your current medications, including over-the-counter products, to avoid drug reactions and ensure your treatment plan stays on track.
Additionally, consider the cost of treatment options, as many are covered by the government’s Pharmaceutical Benefits Scheme (PBS). Consult your doctor or pharmacist to confirm if your medication meets the eligibility criteria for a subsidised price.
Remember that not all treatments work for everyone, so if you don’t see results, discuss this with your dermatologist so they can help you find the right treatment.
2. Action
Ready to speak with your dermatologist?
Use this Discussion Guide to help you prepare for a meaningful conversation with your dermatologist, so you can get the most out of your visit.





